Everything for a better work-care balance

Care 2025 - Higher benefits and more flexibility for care recipients
The year 2025 will bring significant changes in the care sector that will benefit both those in need of care and their relatives. From financial increases to new usage options - here is an overview of the most important changes.
Higher care benefits for more support
From January 1, 2025, care insurance benefits will be increased by 4.5%. This affects both the care allowance for home care by relatives and the care benefits in kind that cover professional care services.
- Care level 2: €347 (care allowance), €796 (benefits in kind)
- Care level 3: €599 (care allowance), €1,497 (benefits in kind)
- Care level 4: €800 (care allowance), €1,859 (benefits in kind)
- Care level 5: €990 (care allowance), €2,299 (benefits in kind)
In addition, the relief amount for care and relief services increases from €125 to €131 per month.
Introduction of the respite budget
From July 2025, a relief budget of €3,539 per year will be introduced. This combines short-term and respite care, giving relatives more flexibility. For young people in need of care up to the age of 25 with care level 4 or 5, an early budget of €3,386 will apply, which can be used from 2024.
Improvements to additional benefits
Further adjustments include:
- Care aids for consumption: increase from €40 to €42 per month.
- Measures to improve the living environment: Increase from €4,000 to €4,180 per person.
- Preventive care: extension to eight weeks and elimination of the previous care period of six months.
Electronic patient file (ePA) brings progress
The electronic patient file (ePA) will be introduced from January 2025. It enables central access to health data and significantly improves the organization and care of people in need of care.
Higher contribution to long-term care insurance
In order to finance these improvements, the contribution rate for long-term care insurance will be increased by 0.2 percentage points. Parents will benefit from graduated rates, while those without children will pay higher contributions.
Summary
The changes to long-term care from 2025 will bring tangible financial improvements, more flexibility and a modern infrastructure. People in need of care and relatives can benefit from these changes and make care even more efficient.
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()

Healthy nutrition in old age - vitality and enjoyment at the same time
A balanced diet is important at every stage of life, but especially in old age it plays a decisive role in health, well-being and quality of life. Which nutrients are particularly important? Which foods should be preferred? And how can you adapt your diet to changing needs? We give you valuable tips for a healthy and enjoyable diet in old age.
1 Why do nutrient requirements change?
As we get older, our metabolism slows down and our energy requirements decrease. At the same time, the need for certain nutrients increases as the body absorbs or processes them less efficiently.
These are particularly important:
- Protein for muscle maintenance
- Calcium and vitamin D for strong bones
- Fiber for healthy digestion
- Omega-3 fatty acids for the heart and brain
- Vitamins and minerals to strengthen the immune system
2. the best foods for a healthy diet in old age
The following foods should be a regular part of your diet to ensure you are optimally nourished:
- Plenty of vegetables and fruit: colorful and varied for a good vitamin supply
- High-quality sources of protein: Fish, eggs, pulses, lean meat or dairy products
- Healthy fats: nuts, olive oil and oily fish such as salmon or mackerel
- Whole grain products: More fiber for regular digestion
- Sufficient fluids: at least 1.5 liters of water or unsweetened tea daily
3. practical tips for everyday life
- Small but nutritious meals: If you have less appetite, focus on high-quality foods.
- Spices instead of salt: Herbs and spices add flavor and aid digestion.
- Regular exercise: Supports the metabolism and improves appetite.
- Eat together: Meals in company increase enjoyment and promote social contact.
4 Conclusion: Nutrition as the key to a vital life
A conscious diet in old age makes a decisive contribution to more energy, mobility and well-being. With a balanced selection of foods and small adjustments in everyday life, the body can be optimally nourished - for a healthy and enjoyable life!
Stay healthy for you and your loved ones and enjoy your meals!
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()

Suddenly needing care – first steps for relatives
A care case often occurs suddenly: after a stay in hospital, a fall or due to a progressive illness. For many relatives, this is the first time they have had to deal with the issue of care. The situation is often characterized by uncertainty, time pressure and emotional stress. This makes it all the more important to know the next steps - without the need to sort everything out immediately.
1. Assess the situation and gain time
The first question to ask is: Is the person in need of care currently safe? Not every decision has to be made immediately. It is often enough to first find a temporary solution and get an overview. Care is not a sprint, but a process.
2. Apply for a care level
A key step is to apply for a care level. This is submitted to the person's care insurance fund and is a prerequisite for financial benefits and support services. The application can be made informally - by telephone or in writing. Important to know: Benefits apply retroactively from the day the application is submitted.
3. record care needs
After the application, an assessment is carried out by the Medical Service. To be well prepared, it helps to document everyday life realistically. This includes mobility, personal hygiene, nutrition, orientation and psychological problems. The whole thing is then measured by the degree of independence. A care diary can help to make the actual need for support visible.
4. Organize support
Care can rarely be managed alone. Depending on the situation, outpatient care services, aids or support from other relatives can provide relief. The right solution is individual and depends on the needs of the person in need of care and the family. There is no one right way.
5. Clarify tasks together and share responsibility
A care case often affects several family members. To avoid being overwhelmed, it is helpful to talk to each other at an early stage. Who can provide regular support? Who will take on organizational tasks? Who will step in if someone is absent?
Open agreements help to clarify expectations and distribute responsibility across several shoulders. It is important to be honest about your own limits. Care doesn't have to be perfectly organized - but it does have to be shared.
6. Take your own stress seriously
A care case does not only affect the person in need of care. Relatives are also faced with new tasks, emotional challenges and organizational pressure. Excessive demands, exhaustion or feelings of guilt are no exception. Seeking support at an early stage is not a sign of weakness, but an important step towards stability.
7. Finding ways together
A care case brings many changes with it - both organizationally and emotionally. Taking a step-by-step approach, sharing tasks and accepting support can provide noticeable relief. No one has to make all the decisions alone or have all the solutions ready.
Care situations often raise complex questions: What services are available? How can care be reconciled with work and everyday life? What support is suitable for the current life situation? This is precisely where the advice offered by benefit at work comes in. In addition to care advice, benefit at work also offers psychosocial support and orientation sessions to relieve the burden on relatives and develop viable solutions together. Accepting help is not a sign of weakness, but an important step towards being able to be there for others in the long term.

Understanding inheritance and wills – creating clarity for tomorrow
Many people are reluctant to deal with the subject of inheritance and wills. It seems complex, emotionally stressful or is put off until later. At the same time, experience shows that if nothing is arranged, relatives often face major organizational and emotional challenges in the event of an emergency. Making provisions therefore does not mean dealing with the end, but taking responsibility - for yourself and for the people who remain. The following steps provide a concise guide to what is important, which documents play a role and how conversations with relatives can be conducted carefully.
1. Get an overview: What has already been arranged?
The first step is to get an overview. Is there already a will? Have precautionary documents been drawn up? And above all: can these be found?
The initial aim is not to rearrange everything, but to know the current status. This clarity alone can be a relief.
2. Create or review a will
A will ensures that your own wishes are carried out. Without a will, the legal order of succession applies - and this does not always correspond to your personal wishes. A handwritten will is generally possible, but should be clearly formulated, dated and signed.
It is also important to review it regularly: life situations change, for example due to marriage, separation, children or the need for care. Provision can grow with you.
3. Compile important documents
An organized folder of documents is a great help for relatives in an emergency. This includes, among other things
- Will
- Lasting power of attorney
- living will
- Care decree
- Overview of accounts, insurance policies and contracts
- Information on digital access
It is often enough to designate a central location and inform relatives about it.
4. Start a conversation with relatives
Many people find it difficult to talk about inheritance and pensions. It is not necessary to discuss all the details. It is often enough to share basic information: What has been arranged? Where are the documents? Who is the contact person?
Such discussions can prevent conflicts and provide security. They can take place in stages - not everything has to be clarified at once.
5. Take your own feelings seriously
This topic touches on issues of finiteness, control and responsibility. Uncertainty, resistance or the need for distance are completely normal. Making provisions is not a one-off act, but a process. Breaks are allowed - the important thing is to start at all.
6. Orientation instead of going it alone
Many people are unsure which steps make sense for their personal situation or how to talk to relatives. Support can provide relief here.
The advice offered by benefit at work provides confidential orientation sessions and psychosocial advice on pension issues, family decisions and stressful life issues. Counseling helps you to gain clarity and be well prepared for the next steps.
Pension provision as a gift to family members
Well-regulated provision takes the pressure off - emotionally and organizationally. It helps relatives to concentrate on the essentials instead of searching for documents or answers in an emergency. Not everything has to be perfect. Every step towards greater clarity is a valuable gift for tomorrow.

Together at one table – making care discussions respectful
When a person becomes in need of care, many things change. In addition to organizational questions, discussions arise that are emotionally charged: Who will take on which tasks? How much support is possible? How can care, work and personal life be reconciled? Care discussions are necessary - and often difficult at the same time. This is precisely why it is important how they are conducted.
One table, many voices, one common goal
Care discussions can help to keep a common picture in mind. You can think of them like a round table: Everyone involved is sitting together, each person bringing their own feelings, concerns and boundaries. A sheet of paper is deliberately placed in the middle of the table - as a symbol of the common goal. For example, this sheet reads:
- The relative in need of care should be well.
- No one should be overburdened.
- Responsibility is shared.
This symbol can be used in a very concrete way - for example as an actual piece of paper on the table. During the conversation, it serves as a reminder of what the core issue is, especially when emotions boil over or conversations descend into accusations.
Why care conversations are often challenging
Caregiving brings with it uncertainty, fear and exhaustion. Old role models resurface, expectations remain unspoken, feelings of guilt interfere with conversations. It is often less about factual issues and more about emotions. Conflicts rarely arise from bad intentions, but from excessive demands. Becoming aware of this is a first step towards greater mutual understanding.
Preparation creates relief
Care discussions are often more constructive if they are not spontaneous or unprepared. It can be helpful to arrange a fixed time and to think about things in advance. Each person involved can answer for themselves:
- What does our relative in need of care currently need?
- What is affordable for me personally and what is not?
- Where do I need support or clear boundaries?
This preparation helps you to stay in touch with yourself and realistically assess your own options. It creates space for exchange instead of justification and reduces the risk of expectations remaining unspoken.
From reproach to a joint solution
Care conversations are not about avoiding conflict, but about conducting them constructively. Differing opinions are normal. It is crucial to keep looking at the page in the middle.
Helpful guiding questions are:
What is sustainable for our family in the long term?
- How can tasks be distributed without overburdening anyone?
- Where do we need external support?
Conflicts can be named. Discussions can also be postponed or conducted in stages. Care is a process and so is coordination. It is important to shift the focus away from apportioning blame and towards joint solutions.
Talk to each other respectfully, even when things get emotional
Care conversations don't have to be perfect. The important thing is that they remain respectful. Simple principles are helpful:
- I-messages instead of accusations
- Name feelings without justifying them
- Allow breaks when it gets too much
- Listen without judging immediately
Phrases such as "I realize that this is overwhelming me right now" or "I want to support, but not alone" create clarity without attacking.
Outside support can provide relief
Sometimes it helps not to have care conversations alone. An external, neutral person can help to structure conversations, classify emotions and keep the focus on the common goal. Preparing for or following up on a conversation can also be a relief.
The advice offered by benefit at work supports family caregivers with guidance - also in preparing for care discussions or clarifying roles, expectations and burdens. A neutral view from the outside can help to open up new perspectives and resolve deadlocked situations.
Acting together in the interests of the relative
The sheet in the middle of the table remains. Conversations can change, as can solutions. Cohesion is created when everyone is seen - the person in need of care as well as the relatives. Care discussions can then become a place where responsibility is shared, burdens are reduced and borne together.

Nursing knowledge compact: What's new in nursing care in 2026
There are also some important changes in care at the start of the new year. The following points provide a compact overview of selected changes that are relevant for family caregivers and people in need of care in everyday life.
- Counseling visits: For care allowance recipients with care levels 2 to 5, proof of two mandatory counseling visits per year (every six months) will be sufficient from 2026, instead of the previous four appointments for care levels 4 and 5. More counseling is still possible and can help to relieve the burden.
- Preventive care: From 2026, preventive care benefits can only be settled for the current and previous calendar year. Anyone claiming benefits for 2026 should therefore submit the statement to the care insurance fund by December 31, 2027.
- Care allowance during hospital or rehab: From 2026, care allowance will continue to be paid for up to eight weeks during hospital, rehab or preventive care stays, instead of only up to four weeks as before. The carer's social security contributions will also continue to be paid during this period.
If you have any questions or are unclear about the changes, the benefit at work care team will be happy to provide individual advice and guidance.

Violence in care - looking, understanding, acting
Violence in care is a sensitive but important topic. Whether in care facilities or at home - excessive demands, time pressure or a lack of training can lead to those in need of care suffering psychologically or physically. How does violence arise in care? What forms does it take? And above all: how can we prevent it?
1 What is violence in care?
Violence in care includes not only physical assaults, but also psychological and structural forms.
These include
- Physical violence: beatings, rough handling, restraints without medical necessity
- Psychological violence: intimidation, humiliation, ignoring needs
- Neglect: Inadequate provision of food, medication or hygiene
- Financial exploitation: Unlawful appropriation of money or valuables
2 Causes and backgrounds
Violence in care often does not arise from malicious intent, but from excessive demands and a lack of support.
Common reasons are:
- Lack of staff and time pressure in care facilities
- Emotional and physical strain on caregiving relatives
- Lack of training and lack of awareness
- Cognitive impairments in those in need of care that make communication difficult
3. how can we recognize violence in care?
Warning signs can be
- Unexplained injuries or hematomas
- Frightened or withdrawn behavior
- Unkempt appearance or malnutrition
- Unusual financial transactions
Caregivers themselves may also show signs of strain, such as irritability or emotional detachment.
4. measures for prevention and intervention
Violence can be prevented if we recognize the problem and actively counteract it:
- Raising awareness and training: caregivers and relatives should be trained to cope with stressful situations.
- More support for family caregivers: Use respite services such as day care or advice centers.
- Better working conditions in care facilities: More staff and a good error culture help to avoid overwork.
- Use reporting centers and contact points: If violence is suspected, relatives and care staff should not remain silent, but contact advice centers or the MDK (Medical Service of the Health Insurance Funds).
5 Conclusion: Taking responsibility - for dignified care
Violence in care is a serious problem that affects us all. Through education, support and open communication, we can help to ensure that those in need of care are cared for in dignity and safety. Let's look together, take action and promote a culture of mindfulness.
Stay vigilant and committed!
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()

In a nutshell: Benefits in kind in nursing care - what does that mean?
Care benefits in kind are care services that are provided directly by an outpatient care service and billed to the care insurance fund. In contrast to care allowance, people in need of care do not receive a cash benefit, but professional support from trained staff.
The benefits in kind include
- Personal hygiene (e.g. washing, showering, dressing)
- Help with household chores (e.g. cleaning, shopping)
- Assistance with nutrition (e.g. meal preparation, food intake)
The care insurance fund covers the costs up to a certain maximum amount, depending on the care level:
- Care level 2 - up to €796 per month
- Care level 3 - up to €1,497 per month
- Care level 4 - up to €1,859 per month
- Care level 5 - up to €2,299 per month
: You can combine benefits in kind and care allowance - this is called a combination benefit. This means that some of the care can be provided by relatives, while a care service provides additional support.
Why are there no benefits in kind for care level 1?
Although people with care level 1 have a recognized need for care, they usually do not yet require regular basic care. Therefore, there are no care benefits in kind for them. Instead, other support benefits are available to them, such as the monthly relief amount of €125 or allowances for care aids.
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()

Home search made easy - Important steps for relatives
Finding a suitable place in a home for a relative in need of care can be a challenge. In view of increasing demand and limited capacity, it is important to take a structured approach and keep key points in mind. With the right preparation and support, you can find the best place for your loved one.
1. clarify needs and wishes
To begin with, you and your relative should consider what requirements and wishes you have for a care home. Is it about special care services, good medical care or proximity to home? The more precisely you define your needs, the better you can search for a suitable place.
2. inform early on
Demand for care places is high, so it's worth starting your search for a home early. Find out about care homes in your region and draw up a list of suitable facilities. Visit the websites of the homes and check available information such as prices, care services and reviews.
3. gain a personal impression
A personal visit to the care homes is essential to get an idea of the atmosphere, the rooms and how residents are treated. Pay attention to how the staff treat the residents, whether the rooms are clean and attractive and whether leisure activities are available. Take the opportunity to ask questions and clarify any outstanding issues.
4. check the financing
The cost of a care place can vary considerably. Clarify in advance what financial resources are available and what support is possible from care insurance companies or other agencies. A discussion with a care advisor can provide helpful guidance here.
5 Registration and waiting lists
As many homes have waiting lists, it is advisable to register with several facilities. Ask how long the waiting time usually is and keep in regular contact with the facilities to increase your chances.
Summary
Finding a place in a care home requires careful planning and patience. There are many steps to consider, from needs analysis to visiting homes and clarifying funding. With a structured approach and early planning, you can ensure the best possible care for your relative.
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()
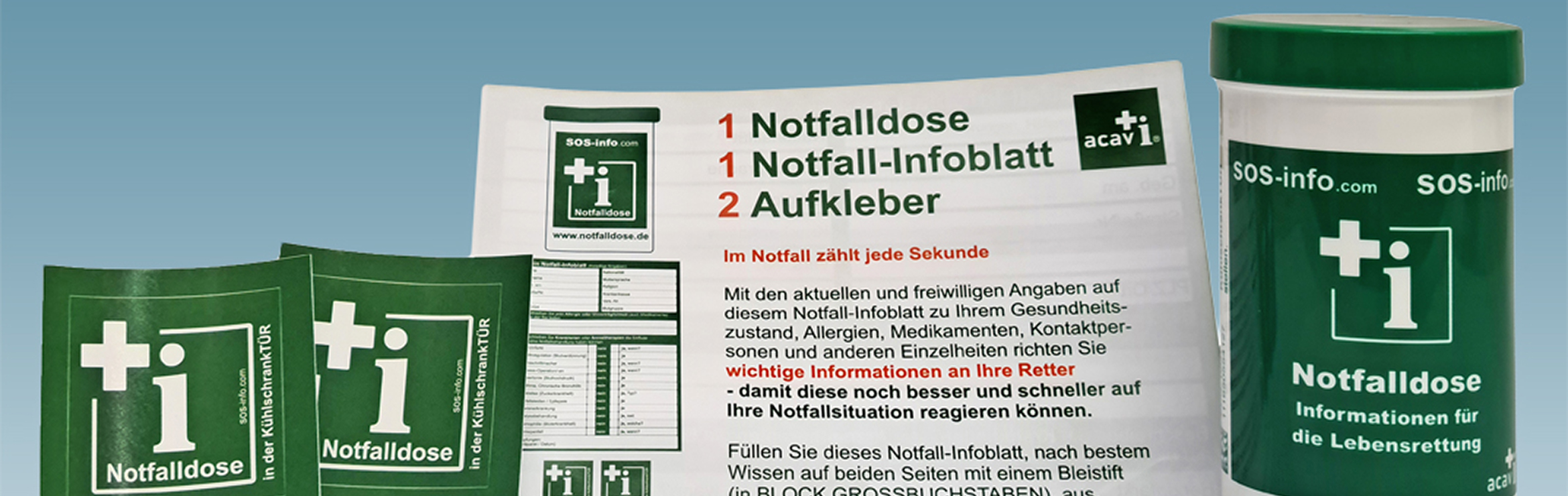
Small box, big help - why the emergency box can save lives
In the day-to-day care of relatives, it is often important to react quickly and correctly in an emergency. A small box can achieve great things: the emergency box. This simple but ingenious tool ensures that all the important information is ready to hand for the emergency services in an emergency. But what exactly is behind it, and why should every family caring for relatives consider using such a box?
What is the emergency box?
The emergency box is a simple plastic box that is kept in the fridge door. It contains an emergency information sheet on which the most important medical data of the person concerned is recorded. This includes
- Pre-existing conditions
- Allergies
- Current medication
- Contact persons in an emergency
The idea behind it: Rescue workers specifically look for the can in the fridge, as this place is present in almost every household and easily accessible. A sticker on the inside of the front door and on the fridge indicates that an emergency box is available.
For whom is the emergency box useful?
The emergency box is particularly helpful for
- Senior citizens who live alone
- People with chronic illnesses or regular medication
- Caring relatives who want to be well prepared for an emergency
- Families who want to ensure that all important information is available in an emergency
Why is the emergency kit so important?
In an emergency, every second counts. Rescue workers often cannot immediately access the necessary information if the person concerned is unconscious or in shock. The emergency box bridges this information gap and gives helpers a clear overview of medical needs.
How does it work?
- The emergency box is filled with a special information sheet containing all the relevant data.
- The box is placed in the refrigerator door - a place that emergency services search as standard.
- Two stickers are affixed: one on the inside of the front door and one on the fridge. They show that an emergency box is available.
Where can I get an emergency box?
Emergency kits are available in pharmacies, from charities such as the German Red Cross and often also in doctors' surgeries. Some organizations offer them free of charge, others charge a small nominal fee.
A small step with a big impact
The emergency box is a simple but effective solution to relieve the burden on people in need of care and their relatives in an emergency. It ensures that emergency services can take the right measures quickly and gives everyone involved a measure of security.
Whether for the care of relatives or for your own household - the emergency box is a small expense with a big impact. And who knows: maybe this little box could save lives one day.
Tip: Think about whether the emergency box could also be a useful gift for elderly relatives or friends. Safety is priceless in an emergency!
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()

Together instead of lonely - How to give older people a Christmas full of joy
For many, Christmas is a time of joy, togetherness and memories. However, it can be a difficult time for older people, especially if they live alone or social contacts have become rare. As a relative, you can do a lot to ensure that the Christmas season is not just filled with nostalgia for your elderly relative, but also with wonderful new moments. It's about creating closeness, alleviating loneliness and integrating small gestures of affection into everyday life.
Why loneliness at Christmas can be so stressful
Old age often brings changes: the loss of a partner, the departure of family members or health restrictions mean that older people feel less involved in the community. This isolation is often particularly painful at Christmas, a time of family celebration. Studies show that loneliness not only affects mental health, but also poses physical risks such as increased blood pressure or heart problems. As a relative, you can make a big difference here by consciously including your elderly relative in the Christmas magic.
Spending time together: Small gestures with a big impact
Even if you don't have time every day, there are numerous ways to create closeness. Plan activities that not only keep your relatives busy, but also actively involve them in the Christmas anticipation. Baking cookies together or decorating the Christmas tree are not only nice traditions, but also offer space for conversations and memories. If your health allows, a trip to the Christmas market can be a real highlight. The smell of roasted almonds and festive music often awaken positive feelings and revive the festive spirit.
Seek out conversation: Reminisce together
Christmas is also a time for stories. Take the opportunity to talk to your older relatives about Christmases past. Ask about old family traditions or anecdotes that you may not yet know yourself. These conversations not only create closeness, but also give older people the feeling that their stories are valued. Even if a face-to-face meeting is not possible, a phone call or video chat can go a long way.
Use local offers and community opportunities
Many seniors feel excluded from social activities due to limited mobility. You can help here by researching local offers. Many communities, churches or senior centers offer Christmas parties, craft groups or singing circles that are specifically designed for older people. Perhaps you can accompany your relatives or organize transport - often all it takes is a little nudge for older people to get involved.
Encourage personal initiative: Actively shape Christmas
Even if it is not always possible to spend personal time together, you can encourage your elderly relatives to actively shape the Christmas season. Writing greeting cards, making decorations or listening to Christmas music are simple ways to enrich everyday life. For some, volunteering, for example in the community, is also a way to experience community and strengthen a sense of purpose.
Christmas doesn't have to be a lonely time for older people. With small gestures, support with activities and the targeted creation of community moments, you can help to bring joy and warmth to this special time of year. Remember: it's often the little things that make the biggest difference. Show affection, listen and give the gift of closeness - this is the greatest gift you can give your elderly relatives.
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()

Watch out for slipping hazards! How older people can get through the winter months safely
The cold season brings special challenges for older people. Snow, ice and wet leaves often turn sidewalks into slippery traps, and a careless step can quickly lead to a fall. However, simple measures can be taken to make the environment safer - both outdoors and within your own four walls. Younger relatives can provide valuable support.
Safe footwear and tread
Non-slip shoes are particularly important for older people in winter. Shoes with a deep tread provide better grip and prevent slipping on slippery surfaces. A regular check of the soles and advice from a specialist retailer will help you choose the right footwear. Family members can provide support here by advising on purchases or replacing old, worn-out shoes.
Visibility in the dark
In winter, the days are shorter and visibility is poorer. Reflective accessories on jackets or a small lamp on a coat can help older people to be clearly visible outdoors. These increase visibility for drivers and other passers-by. Relatives can provide their elderly family members with reflective strips or small lights that can be easily attached to clothing.
Gritting obligation and janitor service
In housing estates and larger residential complexes, a janitor service is often responsible for clearing and gritting the sidewalks. These paths provide safe footing and are ideal for older people. Homeowners must clear and grit the paths themselves in winter to keep them safe - if this is difficult, relatives or neighbors can provide support.
Exercise for balance and stability
Regular walks keep you fit and improve your balance - an important prerequisite for staying safe on your feet and reducing the risk of falls. If you take older family members for walks more often, you support their mobility and fitness. This makes them safer in everyday life and gives them stability.
Safety in your own home
Small measures can also increase safety in your own home. Motion detectors on doors and in the hallway switch the light on automatically when someone enters the room, which is particularly helpful at night. Grab rails in important places, such as in the bathroom or on stairs, provide additional support. Relatives can install these small aids to create a safe home for their elderly family members.
Important tips at a glance:
- Wear non-slip shoes with a good tread
- Reflective clothing or small lights for better visibility
- Only walk on gritted paths if possible
- Regular walks for balance and stability
- Install motion detectors and handholds at home
A little preparation and attention is often all it takes to make the cold season safer for older people. With the support of relatives and small precautions, winter can be enjoyed in a relaxed manner and without fear of slipping.
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()

Understanding blood sugar - How blood sugar levels affect our health
November 14 is World Diabetes Day - an occasion to take a closer look at the topic of blood sugar. Blood sugar levels play a central role in our bodies and have a direct impact on our well-being. But what exactly does "blood sugar" mean, how does the blood sugar balance work and why is a stable blood sugar level so important?
What is blood sugar?
The term "blood sugar" refers to the concentration of glucose in the blood. Glucose is a simple type of sugar and is our body's main source of energy. Everything we eat - especially carbohydrates - is converted into glucose and released into the blood. The cells need glucose to produce energy for all physical and mental functions. In order to channel glucose into the cells, the body needs the hormone insulin, which is produced by the pancreas. A stable blood sugar level ensures that our body is evenly supplied with energy throughout the day.
Why is a stable blood sugar level important?
A constant blood sugar level has many positive effects on health and well-being. A balanced blood sugar level provides more energy, mental clarity and mood stability. Fluctuations in blood sugar levels, on the other hand, for example due to high-sugar snacks or skipping meals, can cause tiredness, irritability and concentration problems. Cravings also occur frequently when blood sugar levels fluctuate greatly.
Long-term fluctuations and high blood sugar levels can pose serious health risks. Constantly elevated blood sugar levels can lead to insulin resistance - a precursor to type 2 diabetes. With insulin resistance, the cells lose their sensitivity to insulin and the blood sugar level remains elevated for longer. This overloads the pancreas as it has to produce more and more insulin to regulate blood sugar. Without timely treatment, insulin resistance can progress to type 2 diabetes and increase the risk of cardiovascular disease, kidney problems and nerve damage.
Tips for a stable blood sugar level
1. eat regular meals: Make sure you eat regularly to avoid sharp fluctuations in blood sugar. Three main meals and, if necessary, small snacks in between ensure a steady supply of energy.
2. balanced diet: Combine carbohydrates with protein and healthy fats. These nutrients slow down the absorption of glucose into the blood and prevent sharp rises and falls in blood sugar.
3. incorporate exercise: Even small bouts of exercise, such as a walk after a meal, help regulate blood sugar levels. Exercise improves the cells' sensitivity to insulin and helps the body to utilize glucose better.
4. avoid sugar and highly processed foods: Refined sugar and processed carbohydrates lead to rapid blood sugar spikes. Focus on whole grain products, vegetables and fiber-rich foods that keep blood sugar levels stable.
A stable blood sugar level is crucial for health and well-being. With a conscious lifestyle, regular exercise and a balanced diet, blood sugar can be kept in balance - an important measure to reduce the risk of diabetes and improve quality of life.
If you would like advice on health or nutrition or suspect that your blood sugar is not in balance, please do not hesitate to consult your GP or take advantage of our advice from benefit at work.
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()

Stress management for family caregivers: an indispensable resource
Caring for relatives is one of the most challenging tasks you can take on in life. Not only does it require time, patience and dedication, but it is often accompanied by emotional and physical stress. It is therefore crucial for family caregivers to actively look after their own wellbeing and develop effective stress management strategies. In this in-depth article, I would like to look at some of the key stressors, as well as specific coping strategies and available support options.
The emotional burden of caregiving: more than just physical exhaustion
In addition to the physical strain of caregiving, the emotional burden is often the biggest stress factor. The constant confrontation with illness and possible progressive deterioration of a loved one's health can lead to a variety of negative emotions, including sadness, fear, guilt and sometimes even anger. Family caregivers can feel emotionally isolated and often feel that they are the only person who can carry the responsibility.
This emotional isolation is reinforced by the "taboo" nature of care work. Many carers are reluctant to talk about their burdens as they feel guilty or are afraid of being seen as "weak" or "failing". This often leads to excessive demands and, in the worst case, to depression and burnout.
How does stress arise?
Stress arises when people feel that a situation is beyond their control and they do not have sufficient coping strategies at their disposal. This can be particularly common in day-to-day care, as the needs of the person in need of care are often unpredictable and the emotional attachment creates additional pressure. This leads to a state of tension that can affect health in the long term
Effects of stress on health
Persistent stress can trigger both mental and physical illnesses. The most common health problems include
- Muscular tension
- tinnitus
- Digestive disorders
- Cardiovascular diseases such as heart attack or stroke
- Mental illnesses such as depression or anxiety disorders
Practical approaches to coping with stress
Organize care tasks better: Structured planning and organization of care can significantly help to reduce stress. It is advisable to draw up a daily or weekly schedule in which not only the care activities but also recovery times are firmly scheduled. This gives relatives a sense of control and allows them to consciously take time for breaks
Create free space: Regular time off is essential in order to be able to survive in long-term care. Options such as respite care or the use of outpatient care services can provide relief. It is important to consciously use these periods for relaxation - be it for sport, hobbies or simply resting
Sleep better: regeneration for body and mind
Sufficient and restful sleep is particularly important for family caregivers in order to cope with the high demands of everyday life. However, sleep disorders are often a problem that results from the physical and mental stress of everyday caring. Interrupted nights, worries and fears about the person in need of care or being constantly on the alert prevent many carers from resting.
Why is sleep so important?
Sleep is a crucial phase of physical and mental regeneration. During this time, the immune system recovers, the brain processes emotions and experiences and the body can recover from the stresses and strains of the day. A lack of restful sleep can significantly impair the ability to take care of yourself and can lead to irritability, concentration problems and even serious health issues.
Tips for better sleep:
- Take regular breaks: schedule fixed times when you can recover from care work, for example by using respite care or night care services.
- Relaxation rituals : Create rituals before going to bed, such as reading a book or listening to calm music, to prepare your body for the rest phase.
- Sleeping environment: Ensure a relaxing and undisturbed sleeping environment, for example by darkening the room, ensuring pleasant temperatures and switching off electronic devices.
- Make use of night care: Use day care services to get relief at night and sleep through the night. This not only gives you much-needed rest, but also ensures that the person in need of care is in good hands.
Do something good for yourself: self-care and mindfulness
Self-care is the key to being able to cope with caring for a relative in the long term. It is important to take regular time out and engage in activities that you enjoy yourself. Family caregivers often put their own needs second, which can lead to exhaustion and burnout in the long run.
Why is self-care so important?
You can only be there for others if you look after and respect yourself sufficiently. Paying attention to your own needs will give you the energy and emotional stability you need to cope with the daily challenges of caregiving.
Tips for self-care:
- Take regular breaks: take small time-outs in your daily routine to recharge your energy. A cup of tea, a walk or simply a few minutes of silence can help you calm down.
- Set rewards: Reward yourself for your work. Whether it's a nice dinner, a visit to the theater or a massage - small rewards are important to motivate yourself and compensate for the efforts of everyday life.
- Maintain hobbies: Don't put your hobbies on hold. Find ways to integrate your interests into your everyday life, be it through sport, music or creative activities. These moments are important sources of relaxation.
- Maintain social contacts: socialize with friends and acquaintances. Social contacts are a valuable balance to everyday care and offer emotional support.
See through the eyes of others:
Change of perspective for more empathy
Another important aspect of stress management for family caregivers is trying to see the situation from the perspective of the person in need of care. Such a change of perspective helps to better understand the needs and feelings of the other person and to develop more patience and empathy.
Why is a change of perspective helpful?
Caring for a loved one can often lead to frustration and misunderstandings. However, if you try to see things from the care recipient's point of view, it often becomes clearer why certain behaviors occur. This can help to avoid conflict and build a more harmonious relationship.
Tips for changing perspective:
- See through the other person's eyes: Try to put yourself in the shoes of the person in need of care and think about what worries, fears or needs they have. Understanding this perspective can help you to react more patiently and empathetically.
- Share feelings: It's important to talk openly about your own feelings too. Share your thoughts and needs with the person in need of care to avoid misunderstandings and promote mutual respect
Support groups: Support through sharing with others
Family caregivers often feel isolated as they have to cope with the challenges of caregiving alone. Support groups offer a valuable opportunity to connect with others in similar situations and find support.
Why are support groups important?
Sharing experiences with other family caregivers can provide relief and reduce feelings of loneliness. In support groups, you can receive valuable tips and advice and find emotional support at the same time.
Advantages of self-help groups:
- Emotional support: here you can talk about your experiences and feel understood as the other participants are going through similar situations.
- Practical advice: Support groups also often offer practical tips and help for everyday caregiving. You can learn from each other and develop new strategies.
- Maintaining social contacts: Self-help groups are also a way of making new social contacts and freeing yourself from isolation.
Defuse crisis situations:
Immediate help for emotional overload
In everyday care work, situations can arise time and again in which the stress becomes too great and emotions boil over. In such crisis situations, it is important to take immediate action to defuse the situation and calm yourself down.
Why do crisis situations arise?
The constant responsibility and intense emotional attachment can escalate in stressful situations. If the demands become too great or the person in need of care reacts unpredictably, many carers feel overwhelmed.
Strategies for defusing crises:
- Leave the room: Remove yourself from the situation for a few minutes to clear your head.
- Deep breathing: Breathe in and out slowly and deeply to calm the body and reduce stress levels.
- Calm your thoughts: Slowly count backwards from ten or repeat a calming phrase such as "I can do this".
- Use your senses: Focus your attention on your surroundings - name five things you see, hear or feel. This mindfulness exercise helps you to anchor yourself in the moment again and view the situation from a calmer perspective
External support options
Family caregivers do not have to cope with caring alone. There are numerous support services that can help you:
Care courses: These offer practical instructions on how to deal with people in need of care and can help to reduce uncertainty in everyday caregiving
Cures for family caregivers: Caregivers who are physically or emotionally stressed have the option of applying for inpatient preventive cures. These offer an opportunity to recover and regain strength.
Care advice: Professional care advisors support family members in organizing care, dealing with legal issues and applying for care services.
Conclusion
Caring for a relative is an emotional and physical challenge that often pushes family caregivers to their limits. Effective stress management is therefore crucial in order to conserve your own energy and stay healthy in the long term. Better sleep, regular self-care, a change of perspective in care, exchanges in self-help groups and dealing with crisis situations in a targeted manner can help family caregivers cope better with their stress and maintain their own quality of life at the same time. It is important to consciously take time for yourself, pay attention to your own needs and make use of support - because this is the only way to ensure that care remains a feasible and fulfilling part of your life in the long term.
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()
Care in the home: what you should bear in mind
The decision to place a family member in a care home is one of the most emotionally difficult a family can make. However, sometimes this choice is unavoidable in order to ensure that people in need of care receive the best possible care and quality of life. Nursing homes offer professional care, medical care and social support that often cannot be provided in home care.
What does nursing home care mean?
Nursing homes, also known as retirement or care homes, are facilities that provide round-the-clock care and support for people in need of care. These homes are designed to meet the physical, mental and emotional needs of their residents. Depending on the health condition and care needs, care homes offer different models of care, from basic care to comprehensive care for those in need of the most intensive care.
Advantages of nursing home care
Nursing homes offer several advantages, especially when home care reaches its limits:
- Round-the-clock professional care: trained nursing staff continuously monitor residents' health and can respond quickly to medical emergencies.
- Medical care: Many homes work closely with doctors, physiotherapists and other healthcare providers to ensure comprehensive medical care.
- Social contact and activities: Care homes offer their residents opportunities to participate in social activities and make new contacts, which can reduce feelings of isolation.
- Relief for relatives: Caring for a family member can be physically and emotionally stressful. A care home can ease this burden and give relatives peace of mind that their loved one is well cared for.
Challenges of nursing home care
Despite the benefits, there are also challenges associated with being placed in a care home:
- Emotional strain: moving into a care home can be emotionally stressful for the person concerned and their family. Getting used to the new environment often takes time and patience.
- Costs: Care homes can be expensive and financing is often a challenge. It is important to find out about various funding options, such as care insurance and state support, at an early stage.
- Loss of autonomy: Residents often have to leave their familiar surroundings and adapt to new routines, which can be perceived as a loss of autonomy.
How do I find the right care home?
Choosing the right care home is crucial for the well-being of the person in need of care. Here are some tips:
- Inform yourself and compare: Use review portals, recommendations from doctors or care advisors and on-site visits to compare different facilities.
- Certifications and quality: Look out for certificates and regular inspections by the Medical Service of the Health Insurance Funds (MDK) that prove the quality of care.
- Care concept and care ratio: Find out about the care concept and care ratio of the home. A high care ratio usually means more intensive care.
- Atmosphere and facilities: Visit the home to assess the cleanliness, care and general atmosphere.
- Conversations with residents and relatives: Talk to current residents and their relatives to gain an insight into satisfaction and care in the home.
Nursing home structure
Nursing homes are divided into different living areas, often with special departments for dementia patients. Each living area has care rooms, care bathrooms, lounges and therapy rooms. In addition to full board, many homes offer individual care and therapy services.
Costs of nursing home care
The costs for accommodation in a nursing home are made up of several components:
- Care costs: partly covered by the care insurance fund, depending on the resident's care level.
- Accommodation and meals: These costs must be borne by the resident.
- Investment costs: These include costs for conversions, modernization and maintenance.
- Additional services: Individual additional services, such as special care measures, may incur additional costs.
Funding and support options
- Care insurance: covers part of the care costs, depending on the resident's care level. There are also benefit supplements depending on the length of stay.
- Care assistance: Support can be applied for from the social welfare office if the resident's own income is insufficient.
- Housing benefit: People in need of care can receive housing benefit under certain conditions.
Conclusion
The decision to move into a care home should not be made hastily. It is important to weigh up all the pros and cons and involve the person in need of care as much as possible in the decision-making process. With the right choice and preparation, accommodation in a care home can enable a dignified and fulfilling life in old age, both for the person in need of care and for their relatives.
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()

Dementia: handling and relief - what is important?
Dementia is one of the most common diseases in old age and poses major challenges for both those affected and their relatives. The right way to deal with people suffering from dementia and ways to relieve the burden on family caregivers are crucial to improving the quality of life of everyone involved. This article provides an overview of important aspects of dealing with dementia and presents relief options for caregivers.
Dealing with people with dementia
Dealing with dementia patients requires empathy, patience and clear communication. People with dementia often experience the world differently and are no longer able to create their own sense of well-being. It is therefore important to take their feelings seriously and accept their world of experience instead of confronting them with reality.
Communication at eye level
A central point in dealing with dementia patients is communication. This should always take place at eye level, which means
- Using simple, short sentences to make it easier to understand what is being said.
- Maintain eye contact and speak calmly, loudly and clearly without shouting.
- Use body language consciously, as non-verbal signals are often better understood than words.
- Instead of open questions, which could overwhelm the person concerned, yes-no questions or simple offers should be made.
- Praise is an important aspect of encouraging positive feelings and boosting self-esteem.
Understand behavior and be patient
People with dementia often behave differently than usual, which can be confusing or frustrating for outsiders. It is important to understand the underlying motivation and to be patient. People with dementia set the pace - excessive demands should be avoided. The following applies: as much help as necessary, but as little as possible.
Relief for relatives
Caring for people with dementia can be very stressful and requires not only physical but also emotional strength. It is therefore essential that family caregivers receive support and relief in order to maintain their own health.
Self-help groups and advice centers
An important step towards relieving the burden is sharing experiences with others in similar situations. Self-help groups offer a valuable platform for sharing experiences and tips. In addition, dementia advice centers and Alzheimer's associations offer professional support and advice. They help with the organization of everyday life, the search for everyday support services and offer training courses that make it easier to deal with dementia patients.
Practical support in everyday life
Family caregivers should not hesitate to take advantage of practical support services. These include:
- Care services that assist with physical care.
- Domestic services that help with the household.
- respite care and short-term care, which allow you to take a break from caring to recharge your batteries.
Contact points in the vicinity
Depending on the federal state, there are specific contact points that offer support, such as the Alzheimer's associations in various regions of Germany. These not only offer advice and training, but also help to find care services.
Improving well-being and quality of life
For people with dementia, it is crucial to convey a feeling of safety and security. This can be achieved through a well-structured daily routine and the creation of positive experiences. Caregivers should take care to create stress-free environments and provide guidance to those affected. It is also important that they have enough time to understand and process information.
Conclusion
Dealing with dementia requires a high degree of empathy and understanding. Family caregivers are often under great pressure and should take advantage of the wide range of support services available to them. Conscious communication, patience and the use of support can significantly improve the quality of life of people with dementia and their relatives. It is important that family caregivers also look after their own health and are not afraid to accept help.
The challenges posed by dementia can be significantly alleviated through caring, respectful treatment and targeted relief. This is the only way that everyone involved can cope with the difficult situation and lead as fulfilling a life as possible despite the illness.
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()

Stroke: symptoms, emergency treatment and prevention
A stroke is a medical emergency that requires immediate attention. It is one of the most common causes of death and is the main reason for permanent disability in adulthood. Every year, around 270,000 people in Germany suffer a stroke, of which almost 200,000 are affected for the first time. However, strokes do not only affect older people - younger people and even children can also be affected. This article presents the most important information on the symptoms, emergency measures and prevention of strokes.
What is a stroke?
A stroke occurs when the blood supply to a part of the brain is interrupted, either by a blockage in a blood vessel (ischemic infarction) or by bleeding in the brain (intracranial hemorrhage). This interruption means that brain cells in the affected area are no longer supplied with sufficient oxygen and nutrients and die within minutes. There are two main types of stroke:
- Ischemic infarction (cerebral infarction): This form of stroke, which accounts for around 75-80% of cases, is caused by a blockage in a blood vessel in the brain, often as a result of an embolism or thrombosis.
- Intracranial hemorrhage (cerebral hemorrhage): In about 15-20% of strokes, a blood vessel in the brain bursts, causing a hemorrhage. This can be caused by high blood pressure or a vascular anomaly.
Symptoms of a stroke
A stroke usually occurs suddenly and causes characteristic symptoms that require immediate medical attention. The most common symptoms are
- Sudden visual disturbances: Loss of vision in one or both eyes or the appearance of double vision.
- Sudden speech or language comprehension disorders: Difficulty finding or understanding words.
- Sudden paralysis or numbness: especially in one side of the body, such as a drooping corner of the mouth or a paralyzed arm.
- Sudden dizziness with unsteady gait: Balance problems or difficulty walking.
- Sudden, very severe headaches: Especially if they occur without any recognizable cause.
Emergency treatment in the event of a stroke
If a stroke is suspected, every minute counts. Acting quickly can save lives and minimize the consequences of a stroke. The so-called FAST test helps to quickly recognize the typical symptoms:
- Face: Ask the person to smile. Is the face contorted on one side? This indicates hemiplegia.
- Arms: Ask the person to stretch both arms forward. In the case of paralysis, both arms cannot be raised or one of the arms drops.
- Speech: Have the person repeat a simple sentence. If they are unable to do this or their speech sounds slurred, there is probably a speech disorder.
- Time: If any of these symptoms occur, call the emergency number 112 immediately - every minute counts!
Prevention of a stroke
Prevention is the best protection against a stroke. Around 70% of strokes could be avoided by adopting a healthy lifestyle. The most important risk factors that need to be controlled are
- High blood pressure: This is the most significant risk factor for a stroke. Regular checks and, if necessary, treatment with medication are essential.
- Cardiac arrhythmia: Atrial fibrillation can promote the formation of blood clots, which can cause a stroke.
- Smoking and alcohol consumption: Smoking and excessive alcohol consumption damage the blood vessels and significantly increase the risk of stroke.
- Diabetes and obesity: Both conditions increase the risk of arteriosclerosis, which can lead to narrowing and hardening of the arteries.
- Poor diet and lack of exercise: An unhealthy diet and too little physical activity promote risk factors such as obesity, high blood pressure and high blood lipid levels.
A healthy lifestyle with regular exercise, a balanced diet, no smoking and a conscious approach to stress can significantly reduce the risk of stroke. For people at increased risk, it is important to have regular check-ups and take any necessary medication consistently.
Conclusion
A stroke is a serious illness that needs to be treated quickly and decisively. Knowing the symptoms and taking the right emergency action can save lives and mitigate the consequences of a stroke. In addition, prevention is the best protection: a healthy lifestyle can reduce many of the risk factors that lead to a stroke. Take care of your health and be prepared for possible emergencies - so that you can act quickly and correctly in an emergency.
Do you have any questions or individual support needs?
Our care advice service is available at any time for further information or individual support needs. You are welcome to arrange a non-binding, personal consultation at:
E-mail pflegeberatung@benefitatwork.de | Telephone consultation 0331 231 879 40 ![]()
